Earlier today, I received an insightful article from Dr. Franceschi discussing the importance of informing patients about the potential long-term consequences of great saphenous vein (GSV) ablation, particularly in relation to arterial bypass surgery. Dr. Franceschi's perspective emphasizes the often-overlooked role of the GSV in future revascularization procedures and highlights the value of CHIVA (Conservative Hemodynamic and Intravenous Treatment for Venous Insufficiency), a minimally invasive approach that preserves the integrity of the GSV while treating varicose veins.
With the increasing prevalence of cardiovascular diseases and the aging population, the great saphenous vein remains a critical autologous graft option for arterial bypass surgeries, including coronary artery bypass grafting (CABG) and lower extremity revascularization. The decision to ablate or "eliminate" the GSV through various methods—such as stripping, endovenous laser treatment (EVLT), radiofrequency ablation (RFA), or sclerotherapy—while effective in managing varicose veins, can significantly impact a patient's future health.
The Critical Role of the Great Saphenous Vein in Arterial Bypass
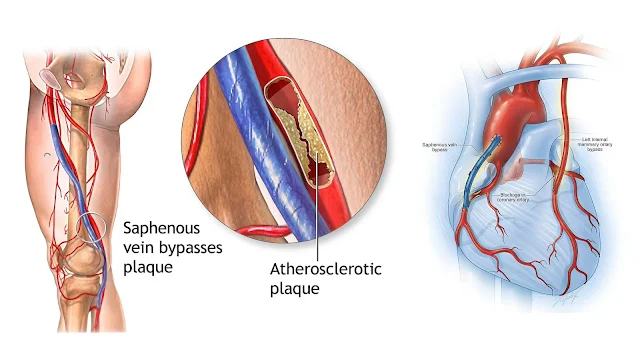
The great saphenous vein is an ideal conduit for bypass procedures due to its size, structure, and durability. In cases of coronary artery disease (CAD) or peripheral artery disease (PAD), where autologous grafts are preferred, the GSV is often the go-to choice for surgeons. The vein's ability to withstand the pressures and stresses of arterial circulation makes it indispensable for high-risk patients who require bypass surgery to restore blood flow to critical areas.
However, when the GSV is ablated for the treatment of varicose veins, this crucial option for arterial grafting is lost. Although endovenous treatments and sclerotherapy are effective at addressing varicose veins, they also result in the irreversible obliteration of the GSV. This poses a significant challenge for patients who may require arterial bypass surgery later in life. Dr. Franceschi's article aptly highlights this concern, calling attention to the need for greater awareness among healthcare providers about the long-term implications of removing this vital vein.
Dr. Franceschi's Perspective: The Value of CHIVA
Dr. Franceschi underscores the importance of CHIVA as a treatment alternative that conserves the great saphenous vein while still addressing the root causes of venous insufficiency. CHIVA is a functional, hemodynamic approach that targets the pathological reflux in the venous system without destroying the vein's integrity. This technique helps preserve the GSV for potential future use, making it an ideal option for patients who may need arterial bypass surgery down the line.
In contrast to traditional ablation techniques, CHIVA focuses on correcting the underlying venous dysfunction by redirecting the blood flow in the saphenous vein, thus avoiding permanent damage. By preserving the GSV, patients maintain access to a valuable graft option for future surgeries, offering them better outcomes should they later require revascularization procedures.
The Role of Modern Interventional Techniques
With the growing popularity of interventional procedures like percutaneous coronary interventions (PCI) and peripheral artery interventions (such as stent placements), there is a common misconception that the need for the great saphenous vein in arterial bypass surgery is diminishing. These modern techniques, particularly in cases of less severe coronary artery disease or peripheral arterial occlusions, can provide effective outcomes without the need for vein grafts.
However, interventional treatments are not suitable for all patients. In complex cases involving multi-vessel coronary artery disease or severe peripheral arterial disease, arterial bypass surgery remains the best option for long-term survival. In such cases, the great saphenous vein continues to be the most preferred and reliable option for bypass grafting.
Therefore, while interventional techniques may reduce the frequency with which the GSV is used, it remains an indispensable resource for many patients requiring complex revascularization. This highlights the importance of carefully considering the long-term health implications of removing the GSV during varicose vein treatments.
The Doctor’s Duty: Transparency and Patient Education
As healthcare providers, it is our responsibility to ensure that patients are fully informed about the potential long-term consequences of removing the great saphenous vein. This includes the possible impact on their future need for arterial bypass surgery. A clear and open discussion about treatment options, including the potential for future cardiovascular procedures, is essential to help patients make informed decisions about their care.



Post a Comment